Osteopath Stephen Haynes looks at the causes of a slipped (herniated) disc as well as new treatment options and simple rehab and prevention exercises you can do at home.
Spinal discs, also called intervertebral discs, sit between the small bones or vertebra of your spine. As these vertebrae are solid, in order for your spine to bend you need healthy discs to provide cushioning, shock absorption and flexibility.
What causes a slipped (herniated) disc?
When a disc slips, herniation can be caused by an injury, such as falling or a collision, causing the disc wall to rupture. More commonly though it happens due to the disc or discs weakening over time, or to twisting movements, poor bending posture or improper lifting, all of which can force the nucleus against an already weakened disc wall.
When the disc wall ruptures or the nucleus even just pushes out a bit, this is called a slipped or herniated disc. Pain can strike immediately, due to the nucleus pressing against a nerve. Additionally, the material of the nucleus irritates the nerve and can worsen the pain.
Your body naturally goes into inflammation mode to try and heal the disc. Inflammation over a short period is a good thing as it’s your body’s healing mechanism, but if pain persists it can mean the inflammation has become a source of pain in itself.
Most people fully recover from a herniated disc and it’s important to get the right advice from a registered professional. The goal of most practitioners is to help get people out of pain and onto a path of long-term wellbeing.

People aged 35-55 are typically most at risk from disc-related back pain, because we tend to become more sedentary and have worsening posture, due to too much sitting.
How common is a slipped (herniated disc)?
People aged 35-55 are typically most at risk from disc-related back pain, although it can affect any age group. This is because as we move past 35, not only can the walls of the discs become weaker and more vulnerable, but we also tend to become more sedentary and have worsening posture, due to too much sitting.
So, while the centres of the discs will still be soft, they can become more at risk of injury or degeneration from reduced physical activity. Luckily, there are a range of lifestyle changes you can make to look after your back and prevent slipped/herniated discs.
How to prevent a slipped (herniated) disc:
Some of the best and simplest ways to look after your discs are:
1. Stay active
Movement is important – if you stay still in one position for too long it puts pressure on one or more of your discs, weakening them over time. Sitting/slouching both cause pressure on the discs at the base of your spine.
2. Maintain good posture
The rule of thumb when standing is to have your ankles, hips, shoulders and ears stacked on top of each other. However, make sure you also hold your body well when you are moving or sitting.
3. Drink plenty of water
Try to drink between one-an-a-half and two litres of water a day as without it, the disc walls can dry out and weaken.
Treatment options for a slipped disc:
Manual Therapy
When someone presents with a herniated disc, manual therapists look at the overall function of the body. They can use stretching techniques to ease the muscle spasm and then use their hands to mobilise the joints. This mobilisation is important to free the movement and allow the body’s natural healing mechanisms to operate.
IDD Therapy
Intervertebral Differential Dynamics Therapy (IDD) is the fastest-growing non-surgical treatment for slipped spinal discs. It’s designed to help people with long-standing disc problems. There are 34 clinics in the UK offering the treatment, which is gentle and non-invasive.
IDD can work on all areas of the spine and helps when manual therapy alone is insufficient to achieve lasting pain relief. The therapy involves a machine that decompresses and mobilises targeted spinal segments. It was developed to address the failings of earlier traction treatment.
You get connected to the machine with a harness, then a pulling force gently opens the space between two vertebrae to relieve pressure on the disc and nerves, all while gentle oscillation mobilises the soft tissues. This combination of decompression and mobilisation helps to take pressure off the troublesome slipped disc and restore mobility.
Slipped disc surgery
Surgery is a last resort for a slipped (herniated) disc, when other manual therapies have not brought about change. Surgery can relieve the leg pain instantly, however, it is not given routinely because there are risks and it does not address the underlying causes of the compression, immobility in the spine and weakness.
Exercise
Once the spine can move again, a therapist can prescribe simple exercises to strengthen the muscles, help support the spine and ease pressure on the disc. Exercise should always be tailored to the individual, based on their condition and ability. Practitioners often use Dr. Stuart Mcgill’s ‘Big Three’ as a starting point (see below), with a mobility exercise to warm up such as the cat-camel move.
Best exercises for slipped disc recovery and prevention
Recover from – or even help prevent – a slipped (herniated) disc with these simple exercises that take just a few minutes a day…
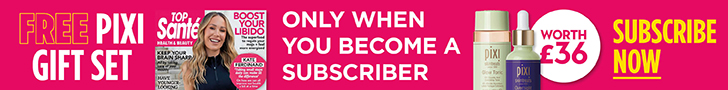
Cat-camel warm-up
- On all fours, slowly arch your spine and hips as much as possible without pain, pulling your tummy in, so your back is in a flexed/rounded position. Your head will hang down. Pause for five secs, breathing slowly.
- Move to the camel position by slowly curving your spine in the opposite direction with your head up, looking to the ceiling.
- Ensure you don’t over-extend or force your spine. Move slowly and carefully, feel the stretch but do not over-stretch. repeat five times.
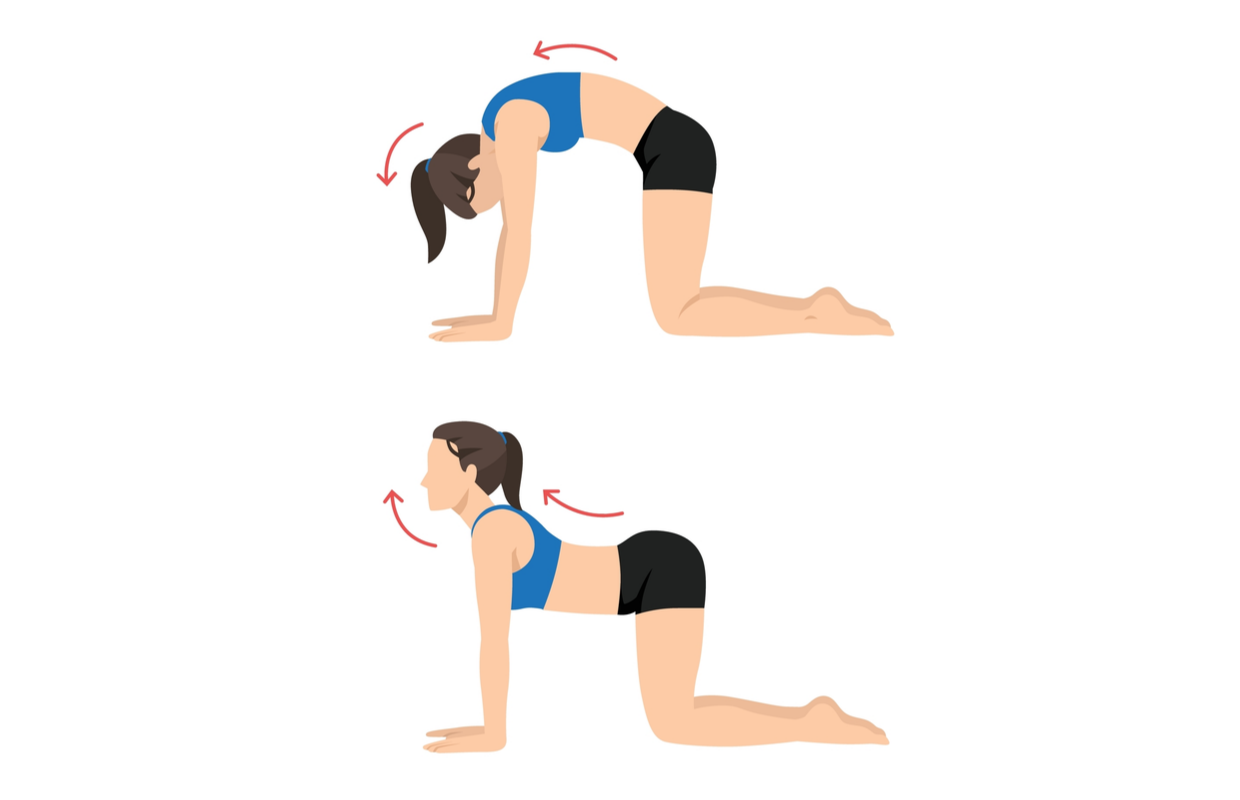
Curl up
- Lie on your back, one leg straight, the other bent, foot flat on the floor.
- Place your palms under the arch of your lower back to maintain the natural curve.
- Slowly raise your head, shoulders and chest together off the floor without bending your lower back at all. keep your elbows on the floor. You won’t come up far. Hold for 3-5 secs, breathing slowly.
- Slowly return to flat position. Do 5-10 reps. to make it harder, lift your elbows off the floor slightly. Try to work your way up to 5-10 second holds. Do three sets of five holds.
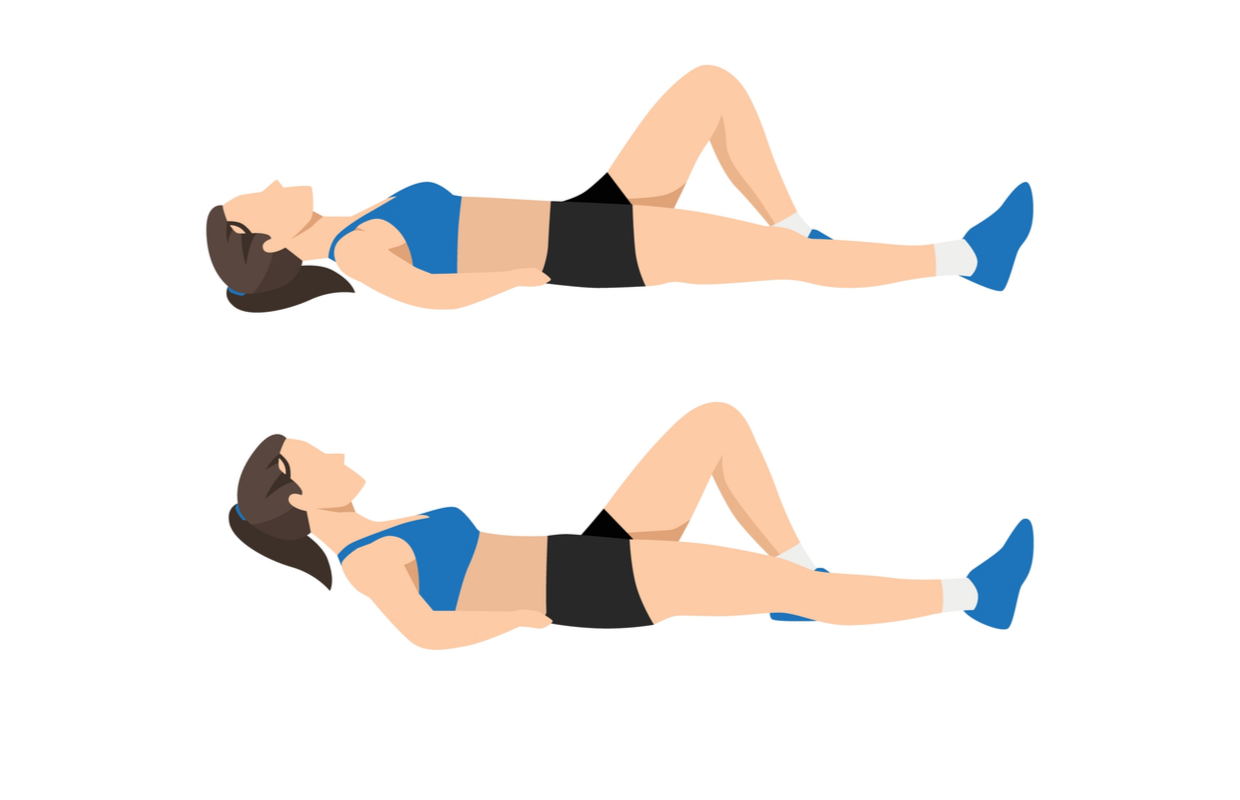
Side plank
Planks stabilise your trunk which supports your spine.
Half side plank:
- Lie on your side with knees bent, feet behind you.
- Lift your hips so only your elbow and knee is in contact with the floor. Put your free hand on your opposite shoulder or on your hip.
- Hold for 10 secs, building up to five sets. Repeat on opposite side.
Full side plank:
- Extend your legs so your body is supported on your elbows and feet. Both feet can contact the floor. Hold for 10 secs.
- Repeat 3-5 times on each side.
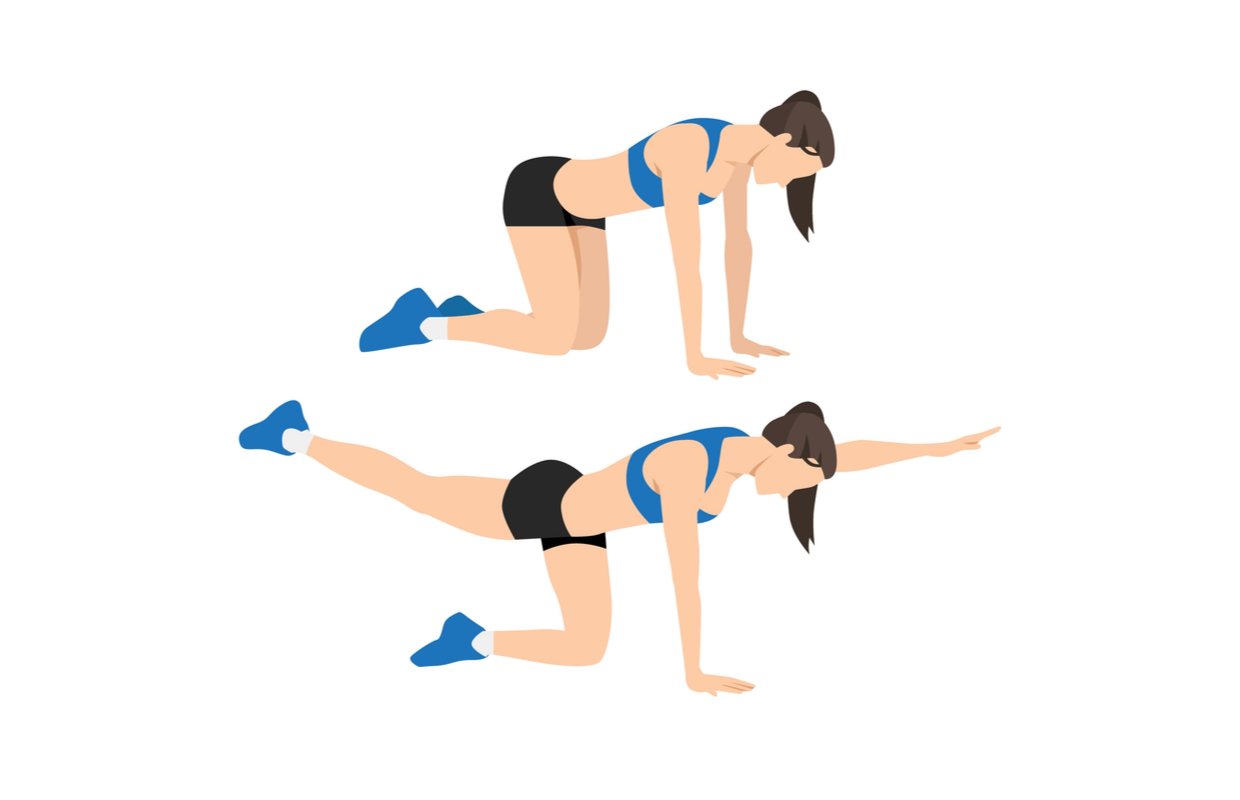
Superman
- Begin on all fours with your hands under your shoulders. Your spine should be in a neutral position i.e. with a slight curve.
- Keep your back still and extend one leg backwards while simultaneously extending the opposite arm forwards until both arm and leg are fully extended. Imagine pushing your heel back as you extend your leg – this will stop your spine from over-arching. Hold for 3-5 secs.
- Swap arms and legs. repeat 5 times, rest, and repeat for 3 sets
Stephen Haynes is an osteopath, IDD therapy provider and clinical director of Active Therapy Clinic in Cirencester, Gloucestershire. Find out more at iddtherapy.co.uk.
Related: Posture workout – 6 exercises to improve your posture at home